Medicine:X-linked hypophosphatemia
| X-linked hypophosphatemia | |
|---|---|
| Other names | X-linked dominant hypophosphatemic rickets, or X-linked Vitamin D-resistant rickets,[1] |
 | |
| This condition is inherited in an X-linked dominant manner. | |
| Complications | osteomalacia (adults), rickets (children), fractures, enthesopathy, spinal stenosis, abnormal gait, short stature, tinnitus, hearing loss, dental complications, in rare exceptions Chiari malformation can occur. |
| Causes | A genetic mutation of the PHEX gene results in elevated FGF23 hormone. |
| Medication | phosphate, vitamin-D or burosumab |
X-linked hypophosphatemia (XLH) is an X-linked dominant form of rickets (or osteomalacia) that differs from most cases of dietary deficiency rickets in that vitamin D supplementation does not cure it. It can cause bone deformity including short stature and genu varum (bow-leggedness). It is associated with a mutation in the PHEX gene sequence (Xp.22) and subsequent inactivity of the PHEX protein.[2] PHEX mutations lead to an elevated circulating (systemic) level of the hormone FGF23 which results in renal phosphate wasting,[3] and locally in the extracellular matrix of bones and teeth an elevated level of the mineralization/calcification-inhibiting protein osteopontin.[4][5] An inactivating mutation in the PHEX gene results in an increase in systemic circulating FGF23, and a decrease in the enzymatic activity of the PHEX enzyme which normally removes (degrades) mineralization-inhibiting osteopontin protein; in XLH, the decreased PHEX enzyme activity leads to an accumulation of inhibitory osteopontin locally in bones and teeth to block mineralization which, along with renal phosphate wasting, both cause osteomalacia and odontomalacia.[6][7]
For both XLH and hypophosphatasia, inhibitor-enzyme pair relationships function to regulate mineralization in the extracellular matrix through a double-negative (inhibiting the inhibitors) activation effect in a manner described as the Stenciling Principle.[8][9] Both these underlying mechanisms (renal phosphate wasting systemically, and mineralization inhibitor accumulation locally) contribute to the pathophysiology of XLH that leads to soft bones and teeth (hypomineralization, osteomalacia/odontomalacia).[10][11][12] The prevalence of the disease is 1 in 20,000.[13]
X-linked hypophosphatemia may be lumped in with autosomal dominant hypophosphatemic rickets under general terms such as hypophosphatemic rickets. Hypophosphatemic rickets are associated with at least nine other genetic mutations.[14] Clinical management of hypophosphatemic rickets may differ depending on the specific mutations associated with an individual case, but treatments are aimed at raising phosphate levels to promote normal bone formation.[15]
Symptoms and signs
The most common symptoms of XLH affect the bones and teeth, causing pain, abnormalities, and osteoarthritis. Symptoms and signs can vary between children and adults and can include:
Children
Adults
- Osteomalacia[16]
- Dental abscesses[20]
- Limited range of movement (enthesopathy)[20] [21]
- Short stature[20]
- Fatigue[19]
- Fractures / pseudofracture[22]
- Bone pain[18] People often have bowed legs or knock knees in which they usually cannot touch both knees and ankles together at the same time.[citation needed]
- Craniostenosis[20]
- Osteoarthritis[23]
- Spinal stenosis[24]
- Hearing loss[20]
- Depression[25]
- Impaired innate immunity[26]
- Defective mineral tessellation (an ultrastructural mineralization deficiency)[27] [28]
Genetics
XLH affects about 1:20,000 individuals and is the most common cause of inherited phosphate wasting.[26]
It is associated with a mutation in the PHEX gene sequence, located on the human X chromosome at location Xp22.2-p22.1.[1][2][29] The PHEX protein regulates another protein called fibroblast growth factor 23 (produced from the FGF23 gene). Fibroblast growth factor 23 normally inhibits the kidneys' ability to reabsorb phosphate into the bloodstream. Gene mutations in PHEX prevent it from correctly regulating fibroblast growth factor 23. The overactivity of FGF-23 reduces vitamin D 1α-hydroxylation and phosphate reabsorption by the kidneys, leading to hypophosphatemia and the related features of ricket.[30] Also in XLH, where PHEX enzymatic activity is absent or reduced, osteopontin[31]—a mineralization-inhibiting secreted substrate protein found in the extracellular matrix of bone[32]—accumulates in bone (and teeth) to contribute to the osteomalacia (and odontomalacia) as shown in the mouse homolog (Hyp) of XLH and in XLH patients.[33][34][35]
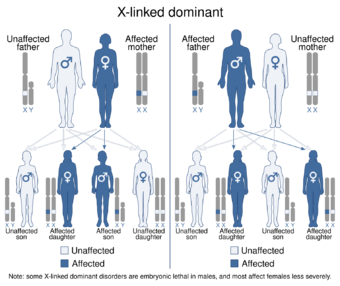
The disorder is inherited in an X-linked dominant manner.[1][2] This means the defective gene responsible for the disorder (PHEX) is located on the X chromosome, and only one copy of the defective gene is sufficient to cause the disorder when inherited from a parent who has the disorder. Males are normally hemizygous for the X chromosome, having only one copy. As a result, X-linked dominant disorders usually show higher expressivity in males than females.[citation needed]
As the X chromosome is one of the sex chromosomes (the other being the Y chromosome), X-linked inheritance is determined by the sex of the parent carrying a specific gene and can often seem complex. This is because, typically, females have two copies of the X-chromosome and males have only one copy. The difference between dominant and recessive inheritance patterns also plays a role in determining the chances of a child inheriting an X-linked disorder from their parentage.[citation needed]
Diagnosis
The clinical laboratory evaluation of rickets begins with assessment of serum calcium, phosphate, and alkaline phosphatase levels. In hypophosphatemic rickets, calcium levels may be within or slightly below the reference range; alkaline phosphatase levels will be significantly above the reference range.Biochemically, XLH is recognized by hypophosphatemia.[36]
Carefully evaluate serum phosphate levels in the first year of life, because the concentration reference range for infants (5.0–7.5 mg/dL) is high compared with that for adults (2.7–4.5 mg/dL).[citation needed]
Serum parathyroid hormone levels are within the reference range or slightly elevated. calcitriol (1,25-(OH)2 vitamin D3) levels are low or within the lower reference range. Most importantly, urinary loss of phosphate is above the reference range.[citation needed]
The renal tubular reabsorption of phosphate (TRP) in X-linked hypophosphatemia is 60%; normal TRP exceeds 90% at the same reduced plasma phosphate concentration. The TRP is calculated with the following formula:[citation needed]
- 1 − [Phosphate Clearance (CPi) / Creatinine Clearance (Ccr)] × 100
Treatment
Conventional therapy consisted of medications including human growth hormone, calcitriol, and oral phosphate,[37][38] and calcitriol;[37][38] Unwanted effects of this therapy have included secondary hyperparathyroidism, nephrocalcinosis, kidney stones, and cardiovascular abnormalities.
In February 2018 the European Medicines Agency first licensed a monoclonal antibody directed against FGF23, the first drug targeting the underlying cause for this condition,[39] called burosumab.[40] It was then licensed by the US Food and Drug Administration in June 2018[41]
The leg deformity can be treated with Ilizarov frames and CAOS.[42] In the event of severe bowing, an osteotomy can be performed to correct the leg shape.[42]
Society and culture
International XLH Alliance – an alliance of international patient groups for individuals affected by XLH and related disorders.
Jennyfer Marques Parinos is a Paralympic bronze medalist from Brazil who has XLH. She competes under a class 9 disability.
See also
- Autosomal dominant hypophosphatemic rickets
- Hypophosphatemia
- Tumor-induced osteomalacia
References
- ↑ 1.0 1.1 1.2 Online Mendelian Inheritance in Man (OMIM) 307800"HYPOPHOSPHATEMIC RICKETS, X-LINKED DOMINANT; XLHR". June 23, 2023. https://omim.org/entry/307800.
- ↑ 2.0 2.1 2.2 Saito, T.; Nishii, Y.; Yasuda, T.; Ito, N.; Suzuki, H.; Igarashi, T.; Fukumoto, S.; Fujita, T. (Oct 2009). "Familial hypophosphatemic rickets caused by a large deletion in PHEX gene". European Journal of Endocrinology 161 (4): 647–651. doi:10.1530/EJE-09-0261. PMID 19581284.
- ↑ Carpenter, TO; Feingold, KR; Anawalt, B; Boyce, A; Chrousos, G; de Herder, WW; Dhatariya, K; Dungan, K et al. (2000). Primary Disorders of Phosphate Metabolism. PMID 25905395.
- ↑ Barros, NM; Hoac, B; Neves, RL; Addison, WN; Assis, DM; Murshed, M; Carmona, AK; McKee, MD (March 2013). "Proteolytic processing of osteopontin by PHEX and accumulation of osteopontin fragments in Hyp mouse bone, the murine model of X-linked hypophosphatemia.". Journal of Bone and Mineral Research 28 (3): 688–99. doi:10.1002/jbmr.1766. PMID 22991293.
- ↑ Boukpessi, T; Hoac, B; Coyac, BR; Leger, T; Garcia, C; Wicart, P; Whyte, MP; Glorieux, FH et al. (February 2017). "Osteopontin and the dento-osseous pathobiology of X-linked hypophosphatemia.". Bone 95: 151–161. doi:10.1016/j.bone.2016.11.019. PMID 27884786.
- ↑ Boukpessi, T.; Hoac, B.; Coyac, B. R.; Leger, T.; Garcia, C.; Wicart, P.; Whyte, M. P.; Glorieux, F. H. et al. (2017). "Osteopontin and the dento-osseous pathobiology of X-linked hypophosphatemia". Bone 95: 151–161. doi:10.1016/j.bone.2016.11.019. PMID 27884786.
- ↑ Barros, N. M.; Hoac, B.; Neves, R. L.; Addison, W. N.; Assis, D. M.; Murshed, M.; Carmona, A. K.; McKee, M. D. (2013). "Proteolytic processing of osteopontin by PHEX and accumulation of osteopontin fragments in Hyp mouse bone, the murine model of X-linked hypophosphatemia". Journal of Bone and Mineral Research 28 (3): 688–699. doi:10.1002/jbmr.1766. PMID 22991293.
- ↑ Reznikov, N.; Hoac, B.; Buss, D. J.; Addison, W. N.; Barros NMT; McKee, M. D. (2020). "Biological stenciling of mineralization in the skeleton: Local enzymatic removal of inhibitors in the extracellular matrix". Bone 138: 115447. doi:10.1016/j.bone.2020.115447. PMID 32454257.
- ↑ McKee, M. D.; Buss, D. J.; Reznikov, N. (2022). "Mineral tessellation in bone and the Stenciling Principle for extracellular matrix mineralization". Journal of Structural Biology 214 (1): 107823. doi:10.1016/j.jsb.2021.107823. PMID 34915130.
- ↑ McKee, MD; Buss, DJ; Reznikov, N (December 13, 2021). "Mineral tessellation in bone and the stenciling principle for extracellular matrix mineralization.". Journal of Structural Biology 214 (1): 107823. doi:10.1016/j.jsb.2021.107823. PMID 34915130.
- ↑ McKee, MD; Hoac, B; Addison, WN; Barros, NM; Millán, JL; Chaussain, C (October 2013). "Extracellular matrix mineralization in periodontal tissues: Noncollagenous matrix proteins, enzymes, and relationship to hypophosphatasia and X-linked hypophosphatemia.". Periodontology 2000 63 (1): 102–22. doi:10.1111/prd.12029. PMID 23931057.
- ↑ Buss, DJ; Reznikov, N; McKee, MD (November 1, 2020). "Crossfibrillar mineral tessellation in normal and Hyp mouse bone as revealed by 3D FIB-SEM microscopy.". Journal of Structural Biology 212 (2): 107603. doi:10.1016/j.jsb.2020.107603. PMID 32805412. https://escholarship.mcgill.ca/concern/articles/vq27zt432.
- ↑ Carpenter TO (Apr 1997). "New perspectives on the biology and treatment of X-linked hypophosphatemic rickets". Pediatr. Clin. North Am. 44 (2): 443–466. doi:10.1016/S0031-3955(05)70485-5. PMID 9130929.
- ↑ Online Mendelian Inheritance in Man (OMIM) 193100
- ↑ "Hypophosphatemic rickets". Genetic and Rare Diseases Information Center. National Institutes of Health. Archived from the original on June 12, 2012. https://web.archive.org/web/20120612101237/http://rarediseases.info.nih.gov/GARD/Disease.aspx?PageID=4&diseaseID=6735. Retrieved October 10, 2012.
- ↑ 16.0 16.1 "Osteomalacia and Rickets". https://www.lecturio.com/concepts/osteomalacia-and-rickets/.
- ↑ Silva, Sandra; Jeanty, Philippe (June 7, 1999). "Cloverleaf skull or kleeblattschadel". TheFetus.net. MacroMedia. http://www.thefetus.net/page.php?id=340.
- ↑ 18.0 18.1 Luger, N. Mach, D. Sevcik, M. Mantyh, P. (2005). Bone cancer pain: From mechanism to model to therapy. Journal of Pain and Symptom Management. 29(5): 32-46.
- ↑ 19.0 19.1 "Fatigue". https://medlineplus.gov/ency/article/003088.htm.
- ↑ 20.0 20.1 20.2 20.3 20.4 Linglart, A.; Biosse-Duplan, M.; Briot, K.; Chaussain, C.; Esterle, L.; Guillaume-Czitrom, S.; Kamenicky, P.; Nevoux, J. et al. (2014). "Therapeutic management of hypophosphatemic rickets from infancy to adulthood". Endocrine Connections 3 (1): R13–R30. doi:10.1530/EC-13-0103. PMID 24550322.
- ↑ Buss, Daniel J.; Rechav, Katya; Reznikov, Natalie; McKee, Marc D. (September 2023). "Mineral tessellation in mouse enthesis fibrocartilage, Achilles tendon, and Hyp calcifying enthesopathy: A shared 3D mineralization pattern". Bone 174: 116818. doi:10.1016/j.bone.2023.116818. ISSN 8756-3282. PMID 37295663. http://dx.doi.org/10.1016/j.bone.2023.116818.
- ↑ "Overview of Bone Fractures". https://www.lecturio.com/concepts/overview-of-bone-fractures/.
- ↑ "Osteoarthritis". https://www.lecturio.com/concepts/osteoarthritis/.
- ↑ Skrinar, A.; Dvorak-Ewell, M.; Evins, A.; MacIca, C.; Linglart, A.; Imel, E. A.; Theodore-Oklota, C.; San Martin, J. (2019). "The Lifelong Impact of X-Linked Hypophosphatemia: Results From a Burden of Disease Survey". Journal of the Endocrine Society 3 (7): 1321–1334. doi:10.1210/js.2018-00365. PMID 31259293.
- ↑ Hawley, S.; Shaw, N. J.; Delmestri, A.; Prieto-Alhambra, D.; Cooper, C.; Pinedo-Villanueva, R.; Javaid, M. K. (2020). "Higher prevalence of non-skeletal comorbidity related to X-linked hypophosphataemia: a UK parallel cohort study using CPRD". Rheumatology 60 (9): 4055–4062. doi:10.1093/rheumatology/keaa859. PMID 33331900.
- ↑ 26.0 26.1 Beck-Nielsen, Signe Sparre; Mughal, Zulf; Haffner, Dieter; Nilsson, Ola; Levtchenko, Elena; Ariceta, Gema; de Lucas Collantes, Carmen; Schnabel, Dirk et al. (February 26, 2019). "FGF23 and its role in X-linked hypophosphatemia-related morbidity". Orphanet Journal of Rare Diseases 14 (1): 58. doi:10.1186/s13023-019-1014-8. ISSN 1750-1172. PMID 30808384.
- ↑ Buss, Daniel J.; Reznikov, Natalie; McKee, Marc D. (November 2020). "Crossfibrillar mineral tessellation in normal and Hyp mouse bone as revealed by 3D FIB-SEM microscopy". Journal of Structural Biology 212 (2): 107603. doi:10.1016/j.jsb.2020.107603. ISSN 1047-8477. PMID 32805412. http://dx.doi.org/10.1016/j.jsb.2020.107603.
- ↑ Buss, Daniel J.; Rechav, Katya; Reznikov, Natalie; McKee, Marc D. (September 2023). "Mineral tessellation in mouse enthesis fibrocartilage, Achilles tendon, and Hyp calcifying enthesopathy: A shared 3D mineralization pattern". Bone 174: 116818. doi:10.1016/j.bone.2023.116818. ISSN 8756-3282. PMID 37295663. http://dx.doi.org/10.1016/j.bone.2023.116818.
- ↑ Online Mendelian Inheritance in Man (OMIM) 300550"PHOSPHATE-REGULATING ENDOPEPTIDASE HOMOLOG, X-LINKED; PHEX". April 18, 2011.
- ↑ Perwad, Farzana; Zhang, Martin Y. H.; Tenenhouse, Harriet S.; Portale, Anthony A. (November 1, 2007). "Fibroblast growth factor 23 impairs phosphorus and vitamin D metabolism in vivo and suppresses 25-hydroxyvitamin D-1alpha-hydroxylase expression in vitro". American Journal of Physiology. Renal Physiology 293 (5): F1577–1583. doi:10.1152/ajprenal.00463.2006. ISSN 1931-857X. PMID 17699549.
- ↑ Sodek, J (2000). "Osteopontin". Critical Reviews in Oral Biology and Medicine 11 (3): 279–303. doi:10.1177/10454411000110030101. PMID 11021631.
- ↑ McKee, MD (2005). "Hierarchies of extracellular matrix and mineral organization in bone of the craniofacial complex and skeleton". Cells Tissues Organs 181 (3–4): 176–188. doi:10.1159/000091379. PMID 16612083.
- ↑ McKee, MD; Hoac, B; Addison, WN; Barros, NM; Millán, JL; Chaussain, C (October 2013). "Extracellular matrix mineralization in periodontal tissues: Noncollagenous matrix proteins, enzymes, and relationship to hypophosphatasia and X-linked hypophosphatemia". Periodontology 2000 63 (1): 102–22. doi:10.1111/prd.12029. PMID 23931057.
- ↑ Boukpessi, T; Hoac, B; Coyac, BR; Leger, T; Garcia, C; Wicart, P; Whyte, MP; Glorieux, FH et al. (November 21, 2016). "Osteopontin and the dento-osseous pathobiology of X-linked hypophosphatemia". Bone 95: 151–161. doi:10.1016/j.bone.2016.11.019. PMID 27884786.
- ↑ Barros, NMT (2013). "Proteolytic processing of osteopontin by PHEX and accumulation of osteopontin fragments in Hyp mouse bone, the murine model of X-linked hypophosphatemia". Journal of Bone and Mineral Research 28 (3): 688–699. doi:10.1002/jbmr.1766. PMID 22991293.
- ↑ Haffner, Dieter; Emma, Francesco; Eastwood, Deborah M.; Duplan, Martin Biosse; Bacchetta, Justine; Schnabel, Dirk; Wicart, Philippe; Bockenhauer, Detlef et al. (July 2019). "Clinical practice recommendations for the diagnosis and management of X-linked hypophosphataemia" (in en). Nature Reviews Nephrology 15 (7): 435–455. doi:10.1038/s41581-019-0152-5. ISSN 1759-507X. PMID 31068690.
- ↑ 37.0 37.1 Imel, E. A.; DiMeglio, L. A.; Hui, S. L.; Carpenter, T. O.; Econs, M. J. (February 15, 2010). "Treatment of X-Linked Hypophosphatemia with Calcitriol and Phosphate Increases Circulating Fibroblast Growth Factor 23 Concentrations". Journal of Clinical Endocrinology & Metabolism 95 (4): 1846–1850. doi:10.1210/jc.2009-1671. PMID 20157195.
- ↑ 38.0 38.1 Glorieux, F. H.; Marie, P. J.; Pettifor, J. M.; Delvin, E. E. (October 30, 1980). "Bone response to phosphate salts, ergocalciferol, and calcitriol in hypophosphatemic vitamin D-resistant rickets". The New England Journal of Medicine 303 (18): 1023–1031. doi:10.1056/NEJM198010303031802. PMID 6252463.
- ↑ Carpenter, TO; Whyte MP; Imel EA; Boot AM; Högler W; Linglart A; Padidela R; Van't Hoff W et al. (May 24, 2018). "Burosumab Therapy in Children with X-Linked Hypophosphatemia". The New England Journal of Medicine 378 (21): 1987–1998. doi:10.1056/NEJMoa1714641. PMID 29791829. https://digitalcommons.wustl.edu/open_access_pubs/6845.
- ↑ "EMA authorisation details". September 17, 2018. https://www.ema.europa.eu/en/medicines/human/EPAR/crysvita#authorisation-details-section.
- ↑ "FDA press release". https://www.fda.gov/news-events/press-announcements/fda-approves-first-therapy-rare-disease-causes-low-phosphate-blood-levels-bone-softening.
- ↑ 42.0 42.1 "X-linked hypophosphatemia | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program" (in en). https://rarediseases.info.nih.gov/diseases/12943/x-linked-hypophosphatemia.
External links
- Hypophosphatemic rickets; XLH; Hypophosphatemia, vitamin D-resistant rickets at NIH's Office of Rare Diseases
| Classification | |
|---|---|
| External resources |
|
 |

